Tendons are a form of connective tissue like ligament tissue but much stronger. They can tolerate very high loads to facilitate the transfer of forces from muscle to bone and also have elastic qualities which allow them to store and release energy. The best example of an energy storage tendon is the Achilles tendon. The Achilles tendon is designed to act like a spring, this happens when we are walking, running, jumping, and cutting.
During the running cycle the Achilles tendon on touch down will stretch and will recoil as we push off. This will allow us to harness the passive energy from the tendon known as the stretch shortening cycle (SSC).
Note: Think of your Achilles tendon like a spring.
What is Achilles Tendinopathy?
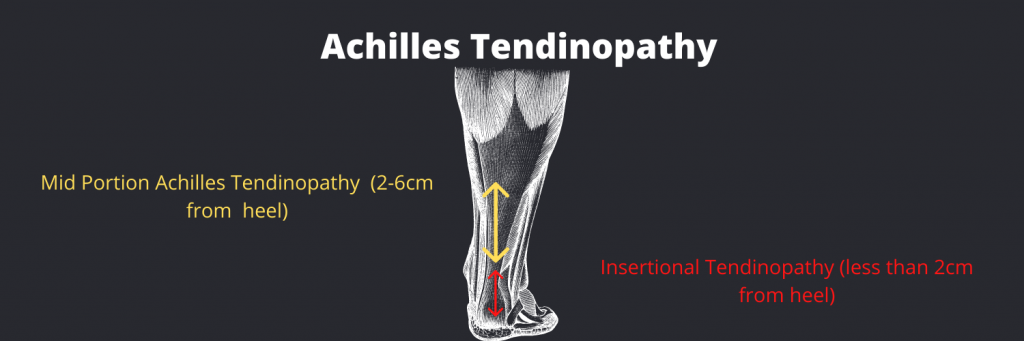
It presents with very localised pain in the middle of the Achilles tendon or the bottom of the Achilles (insertional tendinopathy); often felt during high-load activity such as hopping, running, or jumping and when very irritable it can even be sore with walking. Typically, the pain will present at the start of the activity and warm up (or reduce in intensity) only for the pain to return within a few hours after. The morning after activity the Achilles can often be quite painful and stiff when walking and may take a few hours to settle. This 24-hour pattern is important when it comes to diagnosing a tendinopathy.
As mentioned above we can also have insertional Achilles’ tendon problems where pain will present very local to the calcaneus (heel bone). Insertional Achilles problems are much less likely to tolerate compressive loads, and we must be very careful about compressing the tendon and loading the tendon in the ends of range, especially under heavy load. An example of this is doing heel raises, with or without load, over the edge of a step or calf stretches which add a lot of compression to the insertion site. With the mid-portion Achilles, you don’t really need to be concerned so much about compression, but you need to be careful of increasing pain in the middle part of the tendon, with high loads (running, hopping, jumping).
Note: If you cannot pinpoint your pain with one finger or if your pain moves it is likely not an Achilles tendinopathy
Types of Tendinopathy
Reactive Tendinopathy
A Reactive tendinopathy will usually present in younger people. These tendons usually present with acute pain, no previous history and often a swollen tendon. These patients need a lot of unloading and settling down initially. This phase is a relatively short-term adaptation, this process thickens the tendon to reduce stress and increases the stiffness. On imaging the tendon does appear to be thickened and swollen due to the changes in the proteogycans. This can occur after sudden increased stress or direct impact to the tendon. At this stage, if correctly managed the tendon has the potential to revert to a normal tendon.
Reactive On Degenerative Tendinopathy
These are more common in clinical practice and tend to be in the older population. They may not have recognised the overload they have done but it will be there, so it is important to dig a little bit with your subjective. This population will usually have a history of issues with a very vague loading history. These presentations will be more common in the master’s runner or athlete or very inactive people as they have such poor capacity that very simple things can overload them.
Important Questions that will be covered in a physio assessment.
- Have they done any hill or speed sessions – or started adding these into their current training?
- Have they increased the intensity?
- Have they started to train for a marathon or an event?
- Have they purchased a sport watch like a Garmin or Fitbit? (that can really motivate a patient to do more)
- Have they started preseason after a break?
- Have they transitioned to flat shoes or spikes?
- Changing surfaces that they’re running on – from treadmill to roading running, grass or astroturf?
All these things could be potentially considered a change.

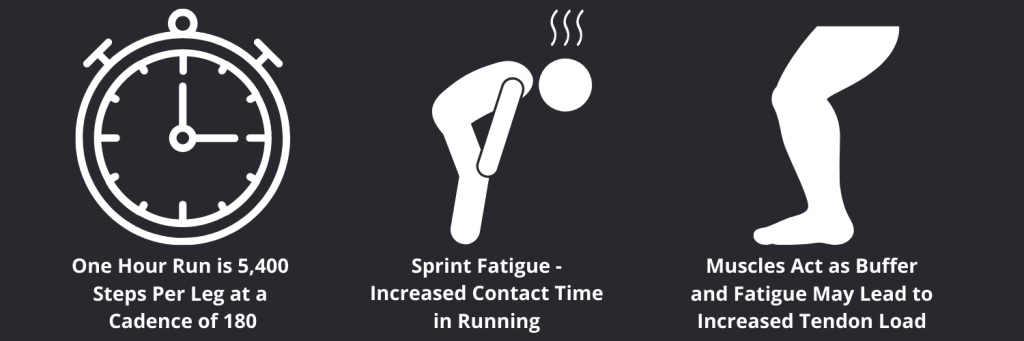
Another thing to consider is fatigue. If you’re running an hour at a cadence of 180, you’re going to take 5400 steps. That can be quite fatiguing for the spring function of your leg. We know Spring function fatigue can lead to changes in the way people run like increased ground contact time which can potentially lead to increased loading of various tissues.
So, muscles act as a buffer and fatigue may increase tendon load which is an important consideration when designing a rehab program.
Achilles Rehabilitation
Firstly, we need to educate our clients as much as possible that tendinopathy’s do not like rest! (Some people do require a period of rest; especially If they’re having a lot of pain, and are intolerant to load, then they may require rest for a brief period, but rest needs to be quantified.) We should not completely rest tendons as they will lose their capacity. Reduce the patient’s load to settle pain and find a less provocative way to load them in the interim.
Load tolerance sets the scene for our assessment for tendinopathy patients. If you can do an activity and the pain is minimal and settles within a day after that activity, then you are generally load tolerant of that activity. We can define acceptable pain by using the numeric pain rating scale or the mild to moderate, severe rating. If its mild that’s considered okay and if its mild to moderate it’s okay (but with caution) and if it’s in the severe pain with an activity or an exercise we have prescribed, then it’s too much and we should stop or else modify that activity. Clinicians can use this to judge if an exercise is appropriate for your tendon’s starting point, but they will also need to assess the capacity of the person, the muscle, the tendon, and the kinetic chain. The clinician will also seek to understand what’s missing in this person’s function and why is this tendon overloaded?
Note: Make sure your clinician finds your adequate baseline and works from there to avoid underloading or overloading
Load management is critical and probably the most important thing we can do to manage people’s pain. Once you have identified how load tolerant a client is, we can start progressive exercise exposure. We can use isometrics if they are not tolerant to isotonic exercise. Additionally if you are in-season, they can be used to reduce pain, develop tolerance in the tendon and maintain strength. Isometrics are also useful in season as they cause the least amount of fatigue.
According to the research, the best way to load a tendon is with heavy slow resistance training to chase the peak loads people are exposed to in their sports. This is where most rehab programs fail as the patients are not being adequately loaded to meet the demands of their sport. Tendon tissue does not respond to these loads very quickly, so we need to apply a high load to these structures over a long period of time (minimum 12 weeks). When we develop a tendinopathy, we lose tendon stiffness and as the tendon acts like a spring, if we want to have a stiffer spring the best way to restore this if through heavy lifting and heavy isometrics. Heavy slow resistance training is vital and must also be done above and below the muscle tendon unit, so not only is the calf complex getting stronger but also the kinetic chain. The tempo is paramount to create time under tension.
After acute heavy exercise there is net loss of collagen production for 24 -36 hours. This means tendons need recovery to allow adaptation, and do not want to be loaded heavy every day. If recovery between training sessions is inadequate it might lead to further injury instead of recovery. Therapeutic loading should be a high magnitude and only performed every other or third day.
One important thing to remember is any load that is slow is not high tendon load, so it is the rate of loading that is important when planning a rehab program. What will limit you is the capacity of the muscle as you will fail quickly at a muscle level but not a tendon level.
For the energy storage capacity of the tendon to be restored heavy slow resistance training and isometrics are typically not enough. Depending on the needs of your patient it is vital to expose them to plyometric load if they are returning to faster activities such as running and jumping. With plyometrics we want to increase the force producing ability of the patient and increase the efficiency of the stretch shortening cycle. Once the patient is load tolerant to hopping, plyometrics should be micro-dosed into their program. When the patient is advancing well with their strength program, they should start velocity or power-based training. This should include fast concentric work that meets the demands of their sport. Starting with double leg and progressing to single leg power work.
Once the patient has successfully returned to sport, it is important that they maintain strength work throughout their athletic career. A maintenance program or some form of specific loading should be continued twice per week for up to 12 months after they have returned to their sport.
Key Points:
· Rest is a prescription
· If pain is low and steady through rehab – the tendon is happy
· Quantify everything
· Tempo work is paramount – fast rate of loading is the most important thing of the tendon.
· Good rehab involves getting people strong and retraining the springs
· Make sure you do not underload your tendon – If unable to progress to the faster stuff it means you haven’t loaded your patient enough
· Prioritise the soleus in rehab